We aim to develop new lines of research and provide health care recommendations and innovative solutions to practitioners in clinical neuropsychology.
Translational approach.
We aim to translate research results into meaningful clinical applications.
Various clinical populations.
Our research focuses on different etiologies, such as Parkinson's disease, cerebellar stroke, as well as COVID-19.
Interdisciplinary Research.
Integrating scientific breakthroughs from relevant disciplines.
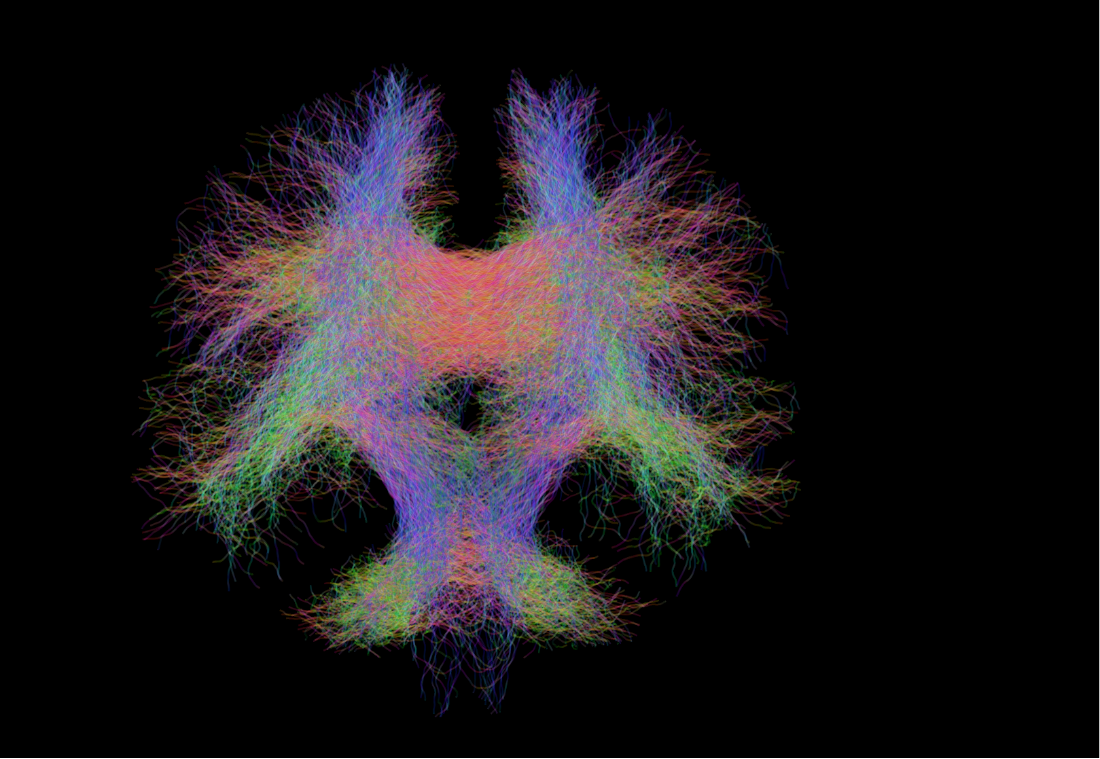
Innovative techniques.
From neuropsychological assessments to neuroimaging, our lab uses diverse methods and techniques for investigating human cognitive and affective functions.
Our mission
More than half of the European population suffers from a neurological condition, such as stroke, dementia or multiple sclerosis (European Academy of Neurology, 2019). Worldwide, neurological disorders are the leading cause of disability and the second leading cause of death (Lancet Neurology, 2019).
The objective of the Clinical and Experimental Neuropsychology laboratory is to improve the quality of life of people living with these diseases. To do so, we pursue four lines of research: i) to increase knowledge of the cerebral bases of cognition, emotion and behavior, (ii) to improve the evaluation and rehabilitation of these processes, (iii) to nourish and reinforce the science-society dialogue, and (iv) to train skilled professionals in the field.

About our lab
The laboratory is currently attached to the Faculty of Psychology and Educational Sciences at the University of Geneva, and enjoys close ties with the Neuropsychology Unit of the Neurology Department at University Hospitals of Geneva (HUG). Moreover, the laboratory is affiliated with two interfaculty centers, the Swiss Center for Affective Sciences and the Swiss Center for the Interdisciplinary study of Gerontology and Vulnerability.
The Unit’s research programme gives students an opportunity to hone their clinical neuropsychology skills and gain experience with clinical populations (primarily adults), while at the same time exploring research questions relating mainly to neuropsychological syndromes and their neuroanatomical substrates–questions that have both theoretical and applied implications.
Meet the team...
The people who make it happen everyday.